7.1 Body Fluids
The body fluid consists of water and substances dissolved in them. There are two types of body fluids, the intracellular fluid present inside the cells and the extracellular fluid present outside the cells. The three types of extracellular fluids are the interstitial fluid or tissue fluid (surrounds the cell), the plasma (fluid component of the blood) and lymph. The blood flowing into the capillary from an arteriole has a high hydrostatic pressure. This pressure is brought about by the pumping action of the blood and it tends to force water and small molecules out through the permeable walls of the capillary into the tissue fluid.
The volume of fluid which leaves the capillary to form tissue fluid is the result of two pressure (hydrostatic pressure and Oncotic pressure). At the anterior end of the capillary bed, the water potential is lesser than hydrostatic pressure inside the capilary bed which is enough to push fluid into the tissues. The tissue fluid has low concentration of protien than that of plasma. At the venous end of the capillary bed, the water potential is greater than the hydrostatic pressure and the fluid from the tissues flows into the capillary and water is drawn back into the blood, taking with it waste products produced by the cells.
Composition of Blood
Blood is the most common body fluid that transports substances from one part of the body to the other. Blood is a connective tissue consisting of plasma (fluid matrix) and formed elements. The plasma constitutes 55% of the total blood volume. The remaining 45% is the formed elements that consist of blood cells. The average blood volume is about 5000ml (5L) in an adult weighing 70 Kg.
7.1.1 Plasma
Plasma mainly consists of water (80-92%) in which the plasma proteins, inorganic constituents (0.9%), organic constituents (0.1%) and respiratory gases are dissolved. The four main types of plasma proteins synthesized in the liver are albumin, globulin, prothrombin and fibrinogen. Albumin maintains the osmotic pressure of the blood. Globulin facilitates the transport of ions, hormones, lipids and assists in immune function. Both Prothrombin and Fibrinogen are involved in blood clotting. Organic constituents include urea, amino acids, glucose, fats and vitamins and the inorganic constituents include chlorides, carbonates and phosphates of potassium, sodium, calcium and magnesium. The composition of plasma is not always constant. Immediately after a meal, the blood in the hepatic portal vein has a very high concentration of glucose as it is transporting glucose from the intestine to the liver where it is stored. The concentration of the glucose in the blood gradually falls after sometime as most of the glucose is absorbed. If too much of protein is consumed, the body cannot store the excess amino acids formed from the digestion of proteins. The liver breaks down the excess amino acids and produces urea. Blood in the hepatic vein has a high concentration of urea than the blood in other vessels namely, hepatic portal vein and hepatic artery.
**Liver receives its blood supply from two sources:** the hepatic artery brings oxygenated blood from the heart, while the hepatic portal vein brings blood from the intestine and other abdominal organs. The blood is re- turned from the liver to the heart by the hepatic veins.
7.1.2 Formed Elements
Red blood cells/corpuscles (erythrocytes), white blood cells/corpuscles (Leucocytes) and platelets are collectively called formed elements.
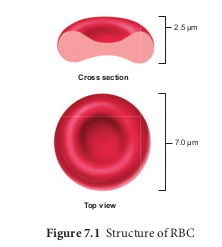
Red Blood Cells
Red blood cells are abundant than the other blood cells. There are about 5 million to 5.5 millions of RBC mm23 of blood in a healthy man and 4.5-5.0 millions of RBC mm23 in healthy women. The RBCs are very small with the diameter of about 7µm (micrometer). The structure of RBC is shown in Figure 7.1. The red colour of the RBC is due to the presence of a respiratory pigment, haemoglobin dissolved in the cytoplasm. Haemoglobin plays an important role in the transport of respiratory gases and facilitates the exchange of gases with the fluid outside the cell (tissue fluid). The biconcave shaped RBCs increases the surface area to volume ratio, hence oxygen diffuses quickly in and out of the cell. The RBCs are devoid of nucleus, mitochondria, ribosomes and endoplasmic reticulum. The absence of these organelles accommodates more haemoglobin thereby maximising the oxygen carrying capacity of the cell. The average life span of RBCs in a healthy individual is about 120 days after which they are destroyed in the spleen (graveyard / cemetery of RBCs) and the iron component returns to the bone marrow for reuse. Erythropoietin is a hormone secreted by the kidneys in response to low oxygen and helps in differentiation of stem cells of the bone marrow to erythrocytes (erythropoiesis) in adults. The ratio of red blood cells to blood plasma is expressed as Haematocrit (packed cell volume).
White Blood Cells
White blood cells (leucocytes) are colourless, amoeboid, nucleated cells devoid of haemoglobin and other pigments. Approximately 6000 to 8000 per cubic mm of WBCs are seen in the blood of an average healthy individual. The different types of WBCs are shown in Figure 7.2. Depending on the presence or absence of granules, WBCs are divided into two types, granulocytes and agranulocytes.
Granulocytes
Granulocytes are characterised by the presence of granules in the cytoplasm and are differentiated in the bone marrow. The granulocytes include neutrophils, eosinophils and basophils.
Neutrophils are also called heterophils or polymorphonuclear (cells with 3-4 lobes of nucleus connected with delicate threads) cells which constitute about 60%- 65% of the total WBCs. They are phagocytic in nature and appear in large numbers in and around the infected tissues.
Eosinophils have distinctly bilobed nucleus and the lobes are joined by thin strands. They are non-phagocytic and constitute about 2-3% of the total WBCs. Eosinophils increase during certain types of parasitic infections and allergic reactions.
Basophils are less numerous than any other type of WBCs constituting 0.5%- 1.0% of the total number of leucocytes. The cytoplasmic granules are large sized, but fewer than eosinophils. Nucleus is large sized and constricted into several lobes but not joined by
delicate threads. Basophils secrete substances such as heparin, serotonin and histamines. They are also involved in inflammatory reactions.
Agranulocytes
Agranulocytes are characterised by the absence of granules in the cytoplasm and are differentiated in the lymph glands and spleen. These are of two types, lymphocytes and monocytes.
Lymphocytes constitute 28% of WBCs. These have large round nucleus and small amount of cytoplasm. The two types of lymphocytes are B and T cells. Both B and T cells are responsible for the immune responses of the body. B cells produce antibodies to neutralize the harmful effects of foreign substances and T cells are involved in cell mediated immunity.
Monocytes (Macrophages) are phagocytic cells that are similar to mast
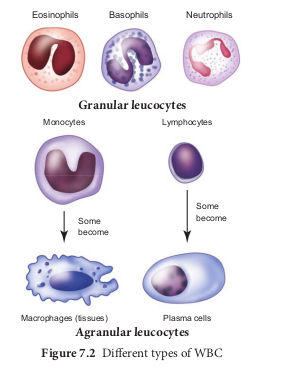
cells and have kidney shaped nucleus. They constitute 1-3% of the total WBCs. The macrophages of the central nervous system are the ‘microglia’, in the sinusoids of the liver they are called ‘Kupffer cells’ and in the pulmonary region they are the ‘alveolar macrophages’.
Platelets
Platelets are also called thrombocytes that are produced from megakaryocytes (special cells in bone marrow) and lack nuclei. Blood normally contains 1, 50,000 -3, 50,000 platelets mm23 of blood. They secrete substances involved in coagulation or clotting of blood. The reduction in platelet number can lead to clotting disorders that result in excessive loss of blood from the body.
7.1.3 Blood Groups
Commonly two types of blood groupings are done. They are ABO and Rh which are widely used all over the world.
ABO Blood Grouping
Depending on the presence or absence of surface antigens on the RBCs, blood group in individual belongs to four different types namely, A, B, AB and O. The plasma of A, B and O individuals have natural antibodies (agglutinins) in them. Surface antigens are called agglutinogens. The antibodies (agglutinin) acting on agglutinogen A is called anti A and the agglutinin acting on agglutinogen B is called anti B. Agglutinogens are absent in O blood group. Agglutinogens A and B are present in AB blood group and do not contain anti A and anti B in them. Distribution of antigens and antibodies in blood groups are shown in Table 7.1. A, B and O are major allelic genes in ABO systems. All agglutinogens contain sucrose, D-galactose, N-acetyl glucosamine and 11 terminal amino acids. The attachments of the terminal amino acids are dependent on the gene products of A and B. The reaction is catalysed by glycosyl transferase.
Distribution of antigens and antibodies in different blood groups
| Bloodgroup | Agglutinogens(antigens) on the RBC | Agglutinin(antibodies)in the plasma |
|---|---|---|
| A | A | Anti B |
| B | B | Anti A |
| AB | AB | No antibodies |
| O | No antigens | Anti A and Anti B |
Rh factor is a protein (D antigen) present on the surface of the red blood cells in majority (80%) of humans. This protein is similar to the protein present in Rhesus monkey, hence the term Rh. Individuals who carry the antigen D on the surface of the red blood cells are Rh1 (Rh positive) and the individuals who do not carry antigen D, are Rh2 (Rh negative). Rh factor compatibility is also checked before blood transfusion. When a pregnant women is Rh2 and the foetus is Rh1 incompatibility (mismatch) is observed. During the first pregnancy, the Rh2 antigens of the foetus does not get exposed to the mother’s blood as both their blood are separated by placenta. However, small amount of the foetal antigen becomes exposed to the mother’s blood during the birth of the first child. The mother’s blood starts to synthesize D antibodies. But during subsequent pregnancies the Rh antibodies from the mother (Rh2) enters the foetal circulation and destroys the foetal RBCs. This becomes fatal to the foetus because the child suffers from anaemia and jaundice. This condition is called erythroblastosis foetalis. This condition can be avoided by administration of anti D antibodies (Rhocum) to the mother immediately after the first child birth.
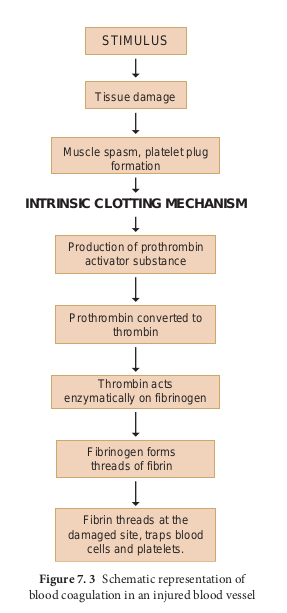
7.1.4 Coagulation of Blood
If you cut your finger or when you get yourself hurt, your wound bleeds for some time after which it stops to bleed. This is because the blood clots or coagulates in response to trauma. The mechanism by which excessive blood loss is prevented by the formation of clot is called blood coagulation or clotting of blood. Schematic representation of blood coagulation is shown Figure 7.3. The clotting process begins when the endothelium of the blood vessel is damaged and the connective tissue in its wall is exposed to the blood. Platelets adhere to collagen fibres in the connective tissue and release substances that form the platelet plug which provides emergency protection against blood loss. Clotting factors released from the clumped platelets or damaged cells mix with clotting factors in the plasma. The protein called prothrombin is converted to its active form called thrombin in the presence of calcium and vitamin K. Thrombin helps in the conversion of fibrinogen to fibrin threads. The threads of fibrins become interlinked into a patch that traps blood cell and seals the injured vessel until the wound is healed. After sometime fibrin fibrils contract, squeezing out a straw-coloured fluid through a meshwork called serum (Plasma without fibrinogen is called serum). Heparin is an anticoagulant produced in small quantities by mast cells of connective tissue which prevents coagulation in small blood vessels.
7.1.5 Composition of Lymph and its Functions
About 90% of fluid that leaks from capillaries eventually seeps back into the capillaries and the remaining 10% is collected and returned to blood system by means of a series of tubules known as lymph vessels or lymphatics. The fluid inside the lymphatics is called lymph. The lymphatic system consists of a complex network of thin walled ducts (lymphatic vessels), filtering bodies (lymph nodes) and a large number of lymphocytic cell concentrations in various lymphoid organs. The lymphatic vessels have smooth walls that run parallel to the blood vessels, in the skin, along the respiratory and digestive tracts. These vessels serve as return ducts for the fluids that are continually diffusing out of the blood capillaries into the body tissues. The end of a vessel is shown in Figure 7.4.
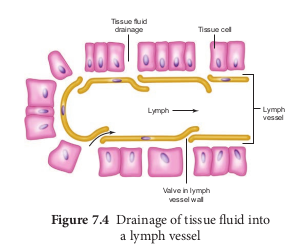
Lymph fluid must pass through the lymph nodes before it is returned to the blood. The lymph nodes that filter the fluid from the lymphatic vessels of the skin are highly concentrated in the neck, inguinal, axillaries, respiratory and digestive tracts. The lymph fluid flowing out of the lymph nodes flow into large collecting duct which finally drains into larger veins that runs beneath the collar bone, the subclavian vein and is emptied into the blood stream. The narrow passages in the lymph nodes are the sinusoids that are lined with macrophages. The lymph nodes successfully prevent the invading microorganisms from reaching the blood stream. Cells found in the lymphatics are the lymphocytes. Lymphocytes collected in the lymphatic fluid are carried via the arterial blood and are recycled back to the lymph. Fats are absorbed through lymph in the lacteals present in the villi of the intestinal wall.
7.2 Blood Vessels – Arteries, Veins and Capillaries
The vessels carrying the blood are of three types; they are the arteries, veins and capillaries. These vessels are hollow structures and have complex walls surrounding the lumen. The blood vessels in humans are composed of three layers, tunica intima, tunica media and tunica externa. The inner layer, tunica intima or tunica interna supports the vascular endothelium, the middle layer, tunica media is composed of smooth muscles and an extra cellular matrix which contains a protein, elastin. The contraction and relaxation of the smooth muscles results in vasoconstriction and vasodilation. The outer layer, tunica externa or tunica adventitia is composed of collagen fibres. The structure of blood vessels is illustrated in Figure 7.5.
Arteries
The blood vessels that carry blood away from the heart are called arteries. The arteries usually lie deep inside the body. The walls of the arteries are thick, non- collapsible to withstand high pressure. Valves are absent and have a narrow lumen. All arteries carry oxygenated blood, except the pulmonary artery. The largest artery, the aorta (2.5 cm in diameter and 2 mm thick) branch into smaller arteries and culminates into the tissues as feed arteries. In the tissues the arteries branches into arterioles. As blood enters an arteriole it may have a pressure of 85 mm Hg (11.3 KPa) but as it leaves and flows into the capillary, the pressure drops to 35 mm Hg (4.7 KPa). (Note 1 mm Hg =0.13 KPa. SI unit of mm Hg is KiloPascal (KPa)). Arterioles

are small, narrow, and thin walled which are connected to the capillaries. A small sphincter lies at the junction between the arterioles and capillaries to regulate the blood supply. Arteries do not always branch into arterioles, they can also form anastomoses.
**What are anastomoses? These are** connections of one blood vessel (ar- teries) with another blood vessel. They provide alternate route of blood flow if the original blood vessel is blocked. For e.g., Arteries in the joints contain nu- merous anastomoses. This allows blood to flow freely even if one of the arteries closes during bending of the joints.
Capillaries
Capillary beds are made up of fine networks of capillaries. The capillaries are thin walled and consist of single layer of squamous epithelium. Tunica media and elastin fibres are absent. The capillary beds are the site for exchange of materials between blood and tissues. The walls of the capillaries are guarded by semilunar valves. The blood volume in the capillaries is high but the flow of blood is slow. Mixed blood (oxygenated and deoxygenated) is present in the capillaries. The capillary bed may be flooded with blood or may be completely bypassed depending on the body conditions in a particular organ.
Why there are no blood capillaries in the cornea of the eye and cartilage? How are these regions supplied with the required nutrients? Suggest why arteries close to the heart have more elastic fibers in their walls than arteries further away from the heart?
Veins
Veins have thinner walls and a larger lumen and hence can be easily stretched. They carry deoxygenated blood except, the pulmonary vein. The blood pressure is low and the lumen has a wide wall which is collapsible. Tunica media is thinner in veins than in arteries. Unidirectional flow of blood in veins is due to the presence of semilunar valves that prevents backflow of blood. Blood samples are usually taken from the veins rather than artery because of low pressure in the veins.
7.2.1 Coronary Blood Vessels
Blood vessels that supply blood to the cardiac muscles with all nutrients and removes wastes are the coronary arteries and veins. Heart muscle is supplied by two arteries namely right and left coronary arteries. These arteries are the first branch of the aorta. Arteries usually surround the heart in the manner of a crown, hence called coronary artery (L. Corona - crown). Right ventricle and posterior portion of left ventricle are supplied by the right coronary artery. Anterior and lateral part of the left ventricle is supplied by the left coronary arteries.
**The Law of Laplace is used to understand the structure and function of blood vessels and the heart.** Laplace law states that the tension in the walls of the blood vessel is proportional to the blood pressure and vessel radius. Blood vessels such as aorta that is subjected to high pressures have thicker walls than the arterioles that are subjected to low pressures.
7.3 Circulatory Pathways
There are two types of circulatory systems, open and closed circulatory systems. Open circulatory system has haemolymph as the circulating fluid and is pumped by the heart, which flows through blood vessels into the sinuses. Sinuses are referred as haemocoel. Open circulatory system is seen in Arthropods and most Molluscs. In closed circulatory system blood is pumped by the heart and flows through blood vessels. Closed circulating system is seen in Annelids, Cephalopods and Vertebrates. All vertebrates have muscular chambered heart. Fishes have two chambered heart. The heart in fishes consists of sinus venosus, an atrium, one ventricle and bulbus arteriosus or conus arteriosus. Single circulation is seen in fishes. Amphibians have two auricles and one ventricle and no inter ventricular septum whereas reptiles except crocodiles have two auricles and one ventricle and an incomplete inter ventricular septum. Thus mixing of oxygenated and deoxygenated blood takes place in the ventricles. This type of circulation is called incomplete double circulation. The left atrium receives oxygenated blood and the right atrium receives deoxygenated blood. Pulmonary and systemic circuits are seen in Amphibians and Reptiles. The Crocodiles, Birds and Mammals have two auricles or atrial chambers and two ventricles, the auricles and ventricles are separated by inter auricular septum and inter ventricular septum. Hence there is complete separation of oxygenated blood from the deoxygenated blood. Pulmonary and systemic circuits are evident. This type of circulation is called complete double circulation.
7.4 Human Circulatory System
The structure of the heart was described by Raymond de viessens, in 1706. Human heart is made of special type of muscle called the cardiac muscle. It is situated in the thoracic cavity and its apex portion is slightly tilted towards left. It weighs about 300g in an adult. The size of our heart is roughly equal to a closed fist. Heart is divided into four chambers, upper two small auricles or atrium and lower two large ventricles. The walls of the ventricles are thicker than the auricles due to the presence of papillary muscles. The heart wall is made up of three layers, the outer epicardium, middle myocardium and inner endocardium.
The space present between the membranes is called pericardial space and is filled with pericardial fluid.
The two auricles are separated by inter auricular septum and the two ventricles are separated by inter ventricular septum The separation of chambers avoids mixing of oxygenated and deoxygenated blood. The auricle communicates with the ventricle through an opening called auriculo ventricular aperture which is guarded by the auriculo ventricular valves. The opening between the right atrium and the right ventricle is guarded by the tricuspid valve (three flaps or cusps), whereas a bicuspid (two flaps or cusps) or mitral valve guards the opening between the left atrium and left ventricle (Figure 7.6). The valves of the heart allows the blood to flow only in one direction, i.e., from the atria to the ventricles and from the ventricles to the pulmonary artery or the aorta. These valves prevent backward flow of blood.
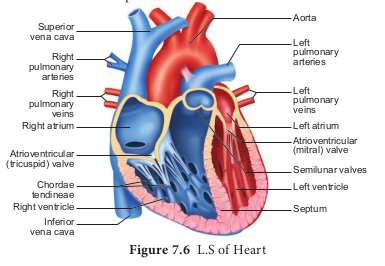
The opening of right and left ventricles into the pulmonary artery and aorta are guarded by aortic and pulmonary valves and are called semilunar valves. Each semilunar valve is made of three half- moon shaped cusps. The myocardium of the ventricle is thrown into irregular muscular ridges called trabeculae corneae. The trabeculae corneae are modified into chordae tendinae. The opening and closing of the semilunar valves are achieved by the chordae tendinae. The chordae tendinae are attached to the lower end of the heart by papillary muscles. Heart receives deoxygenated blood from various parts of the body through the inferior venacava and superior venacava which open into the right auricle. Oxygenated blood from lungs is drained into the left auricle through four pulmonary veins.
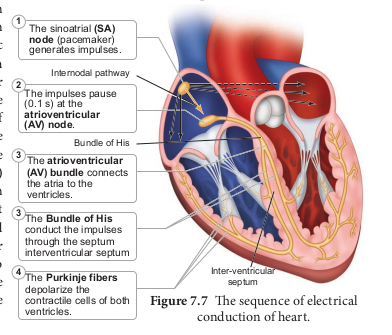
7.4.1 Origin and Conduction of Heart Beat
The heart in human is myogenic (cardiomyocytes can produce spontaneous rhythmic depolarisation that initiates contractions). The sequence of electrical conduction of heart is shown in Figure 7.7. The cardiac cells with fastest rhythm are called the Pacemaker cells, since they determine the contraction rate of the entire heart. These cells are located in the right sinuatrial (SA) node/ Pacemaker. On the left side of the right atrium is a node called auriculo ventricular node (AV node). Two special cardiac muscle fibres originate from the auriculo ventricular node and are called the bundle of His which runs down into the interventricular septum and the fibres spread into the ventricles. These fibres are called the Purkinje fibres.
Pacemaker cells produce excitation through depolarisation of their cell membrane. Early depolarisation is slow and takes place by sodium influx and reduction in potassium efflux. Minimum potential is required to activate voltage gated calcium (Ca+) channels that causes rapid depolarisation which results in action potential. The pace maker cells repolarise slowly via K1 efflux.
HEART BEAT- Rhythmic contraction and expansion of heart is called heart beat. The contraction of the heart is called systole and the relaxation of the heart is called diastole. The heart normally beats 70-72 times per min in a human adult. During each cardiac cycle two sounds are produced that can be heard through a stethoscope. The first heart sound
(lub) is associated with the closure of the tricuspid and bicuspid valves whereas second heart sound (dub) is associated with the closure of the semilunar valves. These sounds are of clinical diagnostic significance. An increased heart rate is called tachycardia and decreased heart rate is called bradycardia.
7.4.2 Cardiac Cycle
The events that occur at the beginning of heart beat and lasts until the beginning of next beat is called cardiac cycle. It lasts for 0.8 seconds. The series of events that takes place in a cardiac cycle.
PHASE 1**: Ventricular diastole**- The pressure in the auricles increases than that of the ventricular pressure. AV valves are open while the semi lunar valves are closed. Blood flows from the auricles into the ventricles passively.
PHASE 2: Atrial systole - The atria contracts while the ventricles are still relaxed. The contraction of the auricles pushes maximum volume of blood to the ventricles until they reach the end diastolic volume (EDV). EDV is related to the length of the cardiac muscle fibre. More the muscle is stretched, greater the EDV and the stroke volume.
PHASE 3: Ventricular systole (isovolumetric contraction) - The ventricular contraction forces the AV valves to close and increases the pressure inside the ventricles. The blood is then pumped from the ventricles into the aorta without change in the size of the muscle fibre length and ventricular chamber volume (isovolumetric contraction).
PHASE 4: Ventricular systole (ventricular ejection) - Increased ventricular pressure forces the semilunar valves to open and blood is ejected out of the ventricles without backflow of blood. This point is the end of systolic volume (ESV).
PHASE 5: (Ventricular diastole) -The ventricles begins to relax, pressure in the arteries exceeds ventricular pressure, resulting in the closure of the semilunar valves. The heart returns to phase 1 of the cardiac cycle.
7.4.3 Cardiac Output
The amount of blood pumped out by each ventricle per minute is called cardiac output(CO). It is a product of heart rate (HR) and stroke volume (SV). Heart rate or pulse is the number of beats per minute. Pulse pressure = systolic pressure – diastolic pressure. Stroke volume (SV) is the volume of blood pumped out by one ventricle with each beat. SV depends on ventricular contraction. CO = HR X SV. SV represents the difference between EDV (amount of blood that collects in a ventricle during diastole) and ESV (volume of blood remaining in the ventricle after contraction). SV = EDV - ESV. According to Frank – Starling law of the heart, the critical factor controlling SV is the degree to which the cardiac muscle cells are stretched just before they contract. The most important factor in stretching cardiac muscle is the amount of blood returning to the heart and distending its ventricles, venous return. During vigorous exercise, SV may double as a result of venous return. Heart’s pumping action normally maintains a balance between cardiac output and venous return. Because the heart is a double pump, each side can fail independently of the other. If the left side of the heart fails, it results in pulmonary congestion and if the right side fails, it results in peripheral congestion. Frank – Starling effect protects the heart from abnormal increase in blood volume.
When blood volume drops down abruptly, what happens to the stroke volume? State whether it increases or decreases?
Blood Pressure
Blood pressure is the pressure exerted on the surface of blood vessels by the blood. This pressure circulates the blood through arteries, veins and capillaries. There are two types of pressure, the systolic pressure and the diastolic pressure. Systolic pressure is the pressure in the arteries as the chambers of the heart contracts. Diastolic pressure is the pressure in the arteries when the heart chambers relax. Blood pressure is measured using a sphygmomanometer (BP apparatus). It is expressed as systolic pressure / diastolic pressure. Normal blood pressure in man is about 120/80mm Hg. Mean arterial pressure is a function of cardiac output and resistance in the arterioles. The primary reflex pathway for homeostatic control of mean arterial pressure is the baroreceptor reflex. The baroreceptor reflex functions every morning when you get out of bed. When you are lying flat the gravitational force is evenly distributed. When you stand up, gravity causes blood to pool in the lower extremities. The decrease in blood pressure upon standing is known as orthostatic hypotension. Orthostatic reflex normally triggers baroreceptor reflex. This results in increased cardiac output and increased peripheral resistance which together increase the mean arterial pressure.
7. 4. 4 Electrocardiogram (ECG)
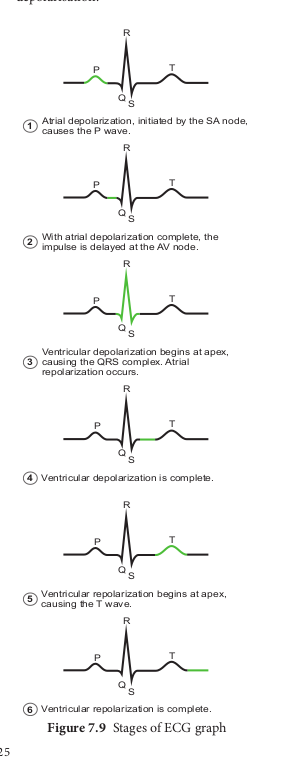
An electrocardiogram (ECG) records the electrical activity of the heart over a period of time using electrodes placed on the skin, arms, legs and chest. It records the changes in electrical potential across the heart during one cardiac cycle. The special flap of muscle which initiates the heart beat is called as sinu-auricular node or SA node in the right atrium. It spreads as a wave of contraction in the heart. The waves of the ECG are due to depolarization and not due to contraction of the heart. This wave of depolarisation occurs before the beginning of contraction of the cardiac muscle. A normal ECG shows 3 waves designated as P wave, QRS complex and T wave as shown in Figure 7.8 and the stages of the ECG graph are shown in Figure 7.9.
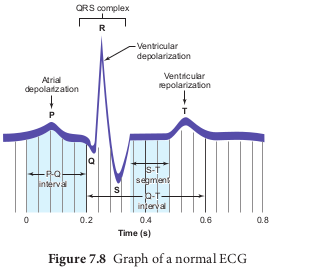
P Wave (Atrial Depolarisation)
It is a small upward wave and indicates the depolarisation of the atria. This is the time taken for the excitation to spread through atria from SA node. Contraction of both atria lasts for around 0.8-1.0 sec.
PQ Interval (AV Node Delay)
It is the onset of P wave to the onset of QRS complex. This is from the start of depolarisation of the atria to the beginning of ventricular depolarisation. It is the time taken for the impulse to travel from the atria to the ventricles (0.12-0.21sec). It is the measure of AV conduction time.
QRS Complex (Ventricular Depolarisation)
No separate wave for atrial depolarisation in the ECG is visible. Atrial depolarisation occurs simultaneously with the ventricular depolarisation. The normal QRS complex lasts for 0.06-0.09 sec. QRS complex is shorter than the P wave, because depolarisation spreads through the Purkinjie fibres. Prolonged QRS wave indicates delayed conduction through the ventricle, often caused due to ventricular hypertrophy or due to a block in the branches of the bundle of His.
ST Segment
It lies between the QRS complex and T wave. It is the time during which all regions of the ventricles are completely depolarised and reflects the long plateau phase before repolarisation. In the heart muscle, the prolonged depolarisation is due to retardation of K+ efflux and is responsible for the plateau. The ST segment lasts for 0.09 sec.
T wave (Ventricular Repolarisation) It represents ventricular repolarisation. The duration of the T wave is longer than QRS complex because repolarisation takes place simultaneously throughout the ventricular depolarisation.
7.5 Double Circulation
Circulation of the blood was first described by William Harvey (1628). There are two types of blood circulation in vertebrates, single circulation and double circulation which is shown in Figure 7.10 (a and b) and 7.11.
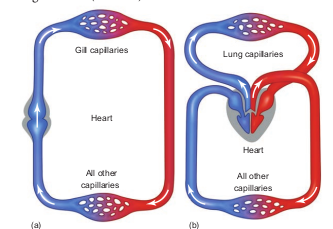
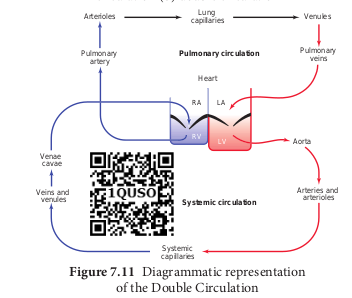
The blood circulates twice through the heart first on the right side then on the left side to complete one cardiac cycle.
The complete double blood circulation is more prominent in mammals because of the complete partition of all the chambers (Auricles and ventricles) in the heart.
In systemic circulation, the oxygenated blood entering the aorta from the left ventricle is carried by a network of arteries,
arterioles and capillaries to the tissues. The deoxygenated blood from the tissue is collected by venules, veins and vena cava and emptied into the right atrium. In pulmonary circulation, the blood from heart (right ventricle) is taken to the lungs by pulmonary artery and the oxygenated blood from the lungs is emptied into the left auricle by the pulmonary vein.
Completely separated circuits have an important advantage. Different pressures are maintained in the pulmonary and systemic circulation. Why is this advantageous? In the lungs the capillaries must be very thin to allow gas exchange, but if the blood flows through these thin capillaries under high pressure the fluid can leak through or ruptures the capillary walls and can accumulate in the tissues. This increases the diffusion distance and reduces the efficiency of the gas exchange. In contrast high pressure is required to force blood through the long systemic circuits. Hence the arteries close to the heart have increased pressure than the arteries
away from the heart. Completely separated circuits (pulmonary and systemic) allow these two different demands to be met with.
7.6 Regulation of Cardiac Activity
The type of heart in human is myogenic because the heart beat originates from the muscles of the heart. The nervous and endocrine systems work together with paracrine signals (metabolic activity) to influence the diameter of the arterioles and alter the blood flow. The neuronal control is achieved through autonomic nervous system (sympathetic and parasympathetic). Sympathetic neurons release nor- epinephrine and adrenal medulla releases epinephrine. The two hormones bind to β – adrenergic receptors and increase the heart rate. The parasympathetic neurons secrete acetylcholine that binds to muscarinic receptors and decreases the heart beat. Vasopressin and angiotensin II, involved in the regulation of the kidneys, results in vasoconstriction while natriuretic peptide promotes vasodilation. Vagus nerve is a parasympathetic nerve that supplies the atrium especially the SA and the AV nodes.
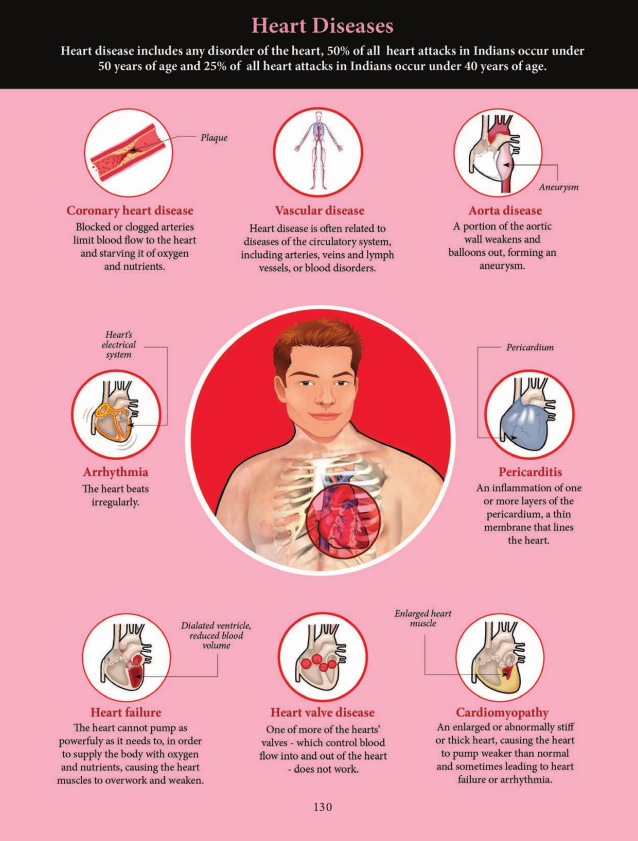
7.7 Disorders of the Circulatory System
Hypertension
Hypertension is the most common circulatory disease. The normal blood pressure in man is 120/80 mmHg. In cases when the diastolic pressure exceeds 90 mm Hg and the systolic pressure exceeds 150 mm Hg persistently, the condition is called hypertension. Uncontrolled hypertension may damage the heart, brain and kidneys.
Coronary Heart Disease
Coronary heart disease occurs when the arteries are lined by atheroma. The build- up of atheroma contains cholesterol, fibres, dead muscle and platelets and is termed Atherosclerosis. The cholesterol rich atheroma forms plaques in the inner lining of the arteries making them less elastic and reduces the blood flow. Plaque grows within the artery and tends to form blood clots, forming coronary thrombus. Thrombus in a coronary artery results in heart attack.
Stroke
Stroke is a condition when the blood vessels in the brain bursts, (Brain haemorrhage) or when there is a block in the artery that supplies the brain, (atherosclerosis) or thrombus. The part of the brain tissue that is supplied by this damaged artery dies due to lack of oxygen (cerebral infarction).
Angina Pectoris
Angina pectoris (ischemic pain in the heart muscles) is experienced during early stages of coronary heart disease. Atheroma may partially block the coronary artery and reduce the blood supply to the heart. As a result, there is tightness or choking with difficulty in breathing. This leads to angina or chest pain. Usually it lasts for a short duration of time.
Myocardial Infarction (Heart Failure)
The prime defect in heart failure is a decrease in cardiac muscle contractility. The Frank- Starling curve shifts downwards and towards the right such that for a given EDV, a failing heart pumps out a smaller stroke volume than a normal healthy heart.
When the blood supply to the heart muscle or myocardium is remarkably reduced it leads to death of the muscle fibres. This condition is called heart attack or myocardial infarction. The blood clot or thrombosis blocks the blood supply to the heart and weakens the muscle fibres. It is also called Ischemic heart disease due to lack of oxygen supply to the heart muscles. If this persists it leads to chest pain or angina. Prolonged angina leads to death of the heart muscle resulting in heart failure.
Rheumatoid Heart Disease
Rheumatic fever is an autoimmune disease which occurs 2-4 weeks after throat infection usually a streptococcal infection. The antibodies developed to combat the infection cause damage to the heart. Effects include fibrous nodules on the mitral valve, fibrosis of the connective tissue and accumulation of fluid in the pericardial cavity.
7.8 Diagnosis and Treatment
Angiogram
Angiogram is a procedure that uses a special dye and X-ray to see how blood flows through the coronary arteries of the heart and it can be used to detect abnormality in the blood vessels through out the body.
Angioplasty
Angioplasty is the stretching of an artery that is narrowed due to atherosclerosis. The risk involved in this procedure is minimal. During an angioplasty a small long balloon catheter is threaded through the blocked artery. A deflated balloon is attached to the catheter and the balloon is inflated to widen the arterial wall. Then the tube and the balloon are removed. A small metal scaffold called stent is left in place. This scaffolding keeps the blood vessel open and allows free flow of blood. Slow releasing stents are now available that can release chemicals to prevent further block of the artery.
Bypass Surgery
When the arteries that bring blood to the heart muscles (coronary artery) are blocked by plaque (accumulation of fat, cholesterol and other substances) the person is advised to undergo Bypass surgery. After the surgery the blood flow to coronary artery is increased and the person is relieved from chest pain. This is a major surgery where damaged blood vessel is replaced by the healthy one taken from different part of the body. Mostly it is taken from legs. During this surgery patients blood system is connected with a pump oxygenator (heart lung machine). After the completion of the surgery the blood vessel is connected to normal the circulation and the blood flows freely.
Heart Transplantation
A heart transplant is a surgical transplantation procedure which is done to replace a diseased or a damaged heart. This procedure is performed on a patient with end stage heart failure or severe coronary artery disease, when other medical ailments or surgical treatments have failed. The most common procedure is to take a functioning heart from a brain dead person (organ donor) and is transplanted in a person with a damaged heart. After the heart transplant the average life span of the person increases.
Cardio Pulmonary Resuscitation (CPR)
In 1956, James Elam and Peter Safar were the first to use mouth to mouth resuscitation. CPR is a life saving procedure that is done at the time of emergency conditions such as when a person’s breath or heart beat has stopped abruptly in case of drowning, electric shock or heart attack. CPR includes rescue of breath, which is achieved by mouth to mouth breathing, to deliver oxygen to the victim’s lungs by external chest compressions which helps to circulate blood to the vital organs. CPR

must be performed within 4 to 6 minutes after cessation of breath to prevent brain damage or death. Along with CPR, defibrillation is also done. Defibrillation means a brief electric shock is given to the heart to recover the function of the heart.
Each year over several million people worldwide die of heart disease, than from other conditions. For some patients heart transplant is the only hope. Raju was 62 years old when muscles of both the ventricles had deteriorated. He was lucky enough because biomedical engineers were able develop a pumping device called ‘total artificial heart’. Raju’s heart was completely removed and an artificial heart was put in place. He was able to go home within a few weeks. This artificial heart would have kept him in alive until suitable real heart was available for transplant.