Mechanism of urine formation in human
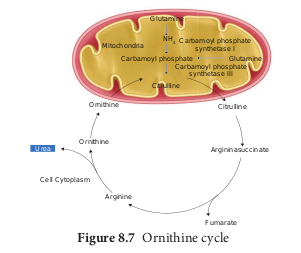
The nitrogenous waste formed as a result of breakdown of amino acids is converted to urea in the liver by the Ornithine cycle or urea cycle (Figure 8.7).
Urine formation involves three main processes namely, glomerular filtration, tubular reabsorption and tubular secretion.
i) Glomerular Filtration: Blood enters the kidney from the renal artery, into the glomerulus. Blood is composed of large quantities of water, colloidal proteins, sugars, salts and nitrogenous end product. The first step in urine formation is the filtration of blood that takes place in the glomerulus. This is called glomerular filtration which is a passive process. The fluid that leaves the glomerular capillaries and enters the Bowman’s capsule is called the glomerular filtrate. The glomerular membrane has a large surface area and is more permeable to water and small molecules present in the blood plasma. Blood enters the glomerulus faster with greater force through the afferent arteriole and leaves the glomerulus through the efferent arterioles, much slower. This force is because of the difference in sizes between the afferent and efferent arteriole (afferent arteriole is wider than efferent arteriole) and glomerular hydrostatic pressure which is around 55mm Hg.
Kidneys produce about 180L of glomerular filtrate in 24 hours. The molecules such as water, glucose, amino acids and nitrogenous substances pass freely from the blood into the glomerulus. Molecules larger than 5nm are barred from entering the tubule. Glomerular pressure is the chief force that pushes water and solutes out of the blood and across the filtration membrane. The glomerular blood pressure (approximately 55 mmHg) is much higher than in other capillary beds. The two opposing forces are contributed by the plasma proteins in the capillaries. These includes, colloidal osmotic pressure (30 mmHg) and the capsular hydrostatic pressure (15 mmHg) due to the fluids in the glomerular capsule. The net filtration pressure of 10 mmHg is responsible for the renal filtration.
Net filtration Pressure = Glomerular hydrostatic pressure - (Colloidal osmotic pressure + Capsular hydrostatic pressure).
Net filtration pressure = 55 mmHg - (30 mmHg + 15 mmHg) 5 = 10mmHg
The effective glomerular pressure of 10 mmHg results in ultrafiltration. Glomerular filtration rate (GFR) is the volume of filtrate formed min21 in all nephrons (glomerulus) of both the kidneys. In adults the GFR is approximately 120- 125mL/min. Blood from the glomerulus is passed out through the efferent arteriole. The smooth muscle of the efferent arteriole contract resulting in vasoconstriction. Table 8.1 shows the relative concentrations of substances in the blood plasma and the glomerular filtrate. The glomerular filtrate is similar to blood plasma except that there are no plasma proteins. In cortical nephrons, blood from efferent arteriole flows into peritubular capillary beds and enters the venous system carrying with it recovered solutes and water from the interstitial fluid that surrounds the tubule.
Table 8.1 Concentration of substances in the blood plasma and in the glomerular filtrate
| Substance | Concentrationin bloodPlasma/g dm-3 | Concentrationin glomerularltrate/g dm-3 |
|---|---|---|
| Water | 900 | 900 |
| Proteins | 80.0 | 0.05 |
| Aminoacids | 0.5 | 0.5 |
| Glucose | 1.0 | 1.0 |
| Urea | 0.3 | 0.3 |
| Uric acid | 0.04 | 0.04 |
| Creatinine | 0.01 | 0.01 |
| Inorganic ions (mainlyNa , K and Cl )1 1 2 | 7.2 | 7.2 |
A person with cirrhosis of the liver has lower than normal levels of plasma proteins and higher than normal GFR. Explain why a decrease in plasma protein would increase GFR.
ii) Tubular Reabsorption
This involves movement of the filtrate back into the circulation. The volume of filtrate formed per day is around 170-180 L and the urine released is around 1.5 L per day, i.e., nearly 99% of the glomerular filtrate that has to be reabsorbed by the renal tubules as it contains certain substances needed by the body. This process is called selective reabsorption. Reabsorption takes place by the tubular epithelial cells in different segments of the nephron either by active transport or passive transport, diffusion and osmosis.
Proximal convoluted Tubule (PCT)- Glucose, lactate, amino acids, Na+ and water in the filtrate is reabsorbed in the PCT. Sodium is reabsorbed by active transport through sodium- potassium (Na+ K+) pump in the PCT. Small amounts of urea and uric acid are also reabsorbed.
Descending limb of Henle’s loop is permeable to water due the presence of aquaporins, but not permeable to salts. Water is lost in the descending limb, hence Na+ and Cl- gets concentrated in the filtrate.
Ascending limb of Henle’s loop is impermeable to water but permeable to solutes such as Na+, Cl- and K+.
The distal convoluted tubule recovers water and secretes potassium into the tubule. Na+, Cl- and water remains in the filtrate of the DCT. Most of the reabsorption from this point is dependent on the body’s need and is regulated by hormones. Reabsorption of bicarbonate (HCO32) takes place to regulate the blood pH. Homeostasis of K+ and Na+ in the blood is also regulated in this region.
Aquaporins are water–permeable channels (membrane transport proteins) that allow water to move across the epithelial cells in relation to the osmotic difference from the lumen to the interstitial fluid.
Collecting duct is permeable to water, secretes K+ (potassium ions are actively transported into the tubule) and reabsorbs Na+ to produce concentrated urine. The change in permeability to water is due to the presence of number of water- permeable channels called aquaporins.
Tubular secretion- Substances such as H+, K+, NH4+, creatinine and organic acids move into the filtrate from the peritubular capillaries into the tubular fluid. Most of the water is absorbed in the proximal convoluted tubule and Na+ is exchanged for water in the loop of Henle. Hypotonic fluid enters the distal convoluted tubule and substances such as urea and salts pass from peritubular blood into the cells of DCT. The urine excreted contains both filtered and secreted substances. Once it enters the collecting duct, water is absorbed and concentrated hypertonic urine is formed. For every H+ secreted into the tubular filtrate, a Na+ is absorbed by the tubular cell. The H+ secreted combines with HCO3-,HPO3- and NH3- and gets fixed as H2CO4+, H2PO4+ and NH4+ respectively. Since H+ gets fixed in the fluid, reabsorption of H+ is prevented.
Osmolarity - The solute concentration of a solution of water is known as the solutions osmolarity, expressed as milliosmoles /liter (mOsm/L)
Formation of concentrated urine Formation of concentrated urine is accomplished by kidneys using counter current mechanisms. The major function of Henle’s loop is to concentrate Na+ and
Cl-. There is low osmolarity near the cortex and high osmolarity towards the medulla. This osmolarity in the medulla is due to the presence of the solute transporters and is maintained by the arrangement of the loop of Henle, collecting duct and vasa recta. This arrangement allows movement of solutes from the filtrate to the interstitial fluid. At the transition between the proximal convoluted tubule and the descending loop of Henle the osmolarity of the interstitial fluid is similar to that of the blood – about 300mOsm.
Ascending and descending limbs of Henle, create a counter current multiplier (interaction between flow of filtrate through the limbs of Henle’s and JMN) by active transport. Figure 8.8 (a) shows the counter current multiplier created by the long loops of Henle of the JM nephrons which creates medullary osmotic gradient.
As the fluid enters the descending limb, water moves from the lumen into the interstitial fluid and the osmolarity of interstitial fluid decreases. To counteract this dilution the region of the ascending limb actively pumps solutes from the lumen into the interstitial fluid and the osmolarity increases to about 1200mOsm in medulla. This mismatch between water and salts creates osmotic gradient in the medulla. The osmotic gradient is also due to the permeability of the collecting duct to urea.
The vasa recta, maintains the medullary osmotic gradient via counter current exchanger (the flow of blood through the ascending and descending vasa recta blood vessels) by passive transport. Figure 8.8 (b) shows counter current exchanger where the vasa recta preserves the medullary gradient while removing reabsorbed water and solutes. This system does not produce an osmotic gradient, but protects the medulla by removal of excess salts from the interstitial fluid and removing reabsorbed water. The vasa recta leave the kidney at the junction between the cortex and medulla. The interstitial fluid at this point is iso-osmotic to the blood.
When the blood leaves the efferent arteriole and enters vasa recta the osmolarity in the medulla increases (1200mOsm) and
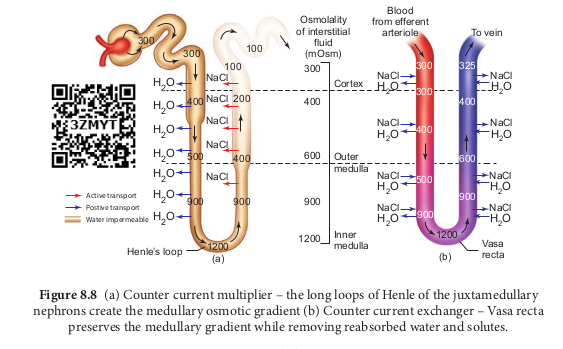
results in passive uptake of solutes and loss of water in descending vasa recta. As the blood enters the cortex, the osmolarity in the blood decreases (300mOsm) and the blood loses solutes and gains water.
At the final stage in collecting duct to form concentrated urine (hypertonic). Human kidneys can produce urine nearly four times concentrated than the initial filtrate formed.
List the pathways involved in the homeostatic compensation in case of severe dehydration.