Chapter 4 Sterilization Chapter Outline
4.1 Need for Sterilization
4.2 Methods of Sterilization
4.3 Physical Methods of Sterilization
4.4 Sterilization by Heat
4.5 Radiation
4.6 Filtration
After studying this chapter the student will be able,
• To understand the concepts of sterilization to maintain aseptic conditions.
• To compare the effectiveness of dry heat (red heat, flamimg, incineration, hot air oven), and moist heat (boiling, autoclaving, pasteurization).
• To learn the uses of pasteurization in the field of food industry.
• To describe the role of radiation in killing pathogens.
• To describe how separation of microor- ganism is achieved through filtration.
Learning Objectives
Microorganisms are ubiquitous. They can contaminate, infect or decay inorganic and organic matter. Hence, it becomes necessary to kill or remove them from materials or from areas around us. This is the objective of sterilization.
oth aft
The process of sterilization is used in Microbiology • for preventing contamination by
extraneous organisms • in surgery for maintaining asepsis • in food and drug manufacture for
ensuring safety from contaminating organisms
The choice of methods of sterilization depend on the purpose for which it is carried out: the material to be sterilized and the nature of the microorganisms that are to be removed or destroyed.
The inoculation loop is sterilized with flame or any er heat source, until it becomes red hot before and
er each use.
As early as the stone age, humans used physical methods of microbial control to preserve foods,
like drying (desiccation) and salting (osmotic pressure).
Sterilization is defined as the process of complete removal or destruction of all forms of microbial life, including vegetative cells and their spores.
Need for Sterilization
The aim of all sterilization strategies is to kill or remove the unwanted microorganisms. In certain cases, microbes are regarded as potential pathogens and therefore it is essential to eliminate these forms (vegetative and spores) of microbial life. All microbiological techniques require appropriate and adequate sterilization.
Sterilization of culture media, containers and instruments is essential in microbiological work for isolation and maintenance of microorganisms. In surgery and medicine, the sterilization of instruments, drugs and other supplies is important for the prevention of infection.
Flowchart 4.1: Physical
• Infrare • Ultravi
• Red heat • Flaming • Incineration • Hot air oven
• Temperature below 100°C
• Temperature at 100°C
• Temperature above 100°C
Moist heatDry heat
Heat
Physical m
Non ioni
Methods of Sterilization
Growth and multiplication of microorganisms can be controlled by removing, killing or inhibiting them using various physical or chemical agents.
Physical Methods of Sterilization
The various physical methods of sterilization are given in flowchart 4.1
Sterilization by Heat
Heat is the most rapid and best method of sterilization. It is the method of choice that the material to be sterilized is stable enough to withstand the required temperature necessary to kill the microbes. The time needed for sterilization depends on the initial number of organisms present, type of materials to be sterilized (hence washed and cleaned items are easier to sterilize than dirty ones) and also on the temperature used. Spores need higher temperatures while vegetative bacteria can be destroyed at lower temperatures.
Methods of Sterilization
d olet
ethods
• X-rays • Gamma rays
Radiation
• Depth filter • Membrane filter • Air filter
Filtration
Ionizing zing
Heating process in canning was first used by Nicholas Appert in 1890. He described a safe means of preserving all kinds of food substances in containers or in cans. Appert is known as father of cannning.
Infobits
Heat resistance varies among different microorganisms. These differences can be expressed in terms of thermal death point. Thermal Death Point (TDP) is the lowest temperature at which all the microorganisms in a particular liquid suspension will be killed in 10 minutes.
Another factor to be considered in sterilization is the duration of time required. This is expressed as Thermal Death Time (TDT). TDT is the minimal time required for all microorganism in a particular liquid culture to be killed at a given temperature. Both TDP and TDT are useful guidelines that indicate the degree of treatment required to kill a given population of bacteria.
Decimal Reduction Time (DRT) is related to bacterial heat resistance. DRT is the time, in minutes, in which 90% of a population of microorganism at a given temperature will be killed.
Heat is employed either as dry heat or moist heat.
Sterilization by Dry Heat
Dry heat is frequently used for the sterilization of glassware and laboratory equipments. In dry heat sterilization, microbial cells are apparently killed by oxidation of their constituents and protein denaturation. Dry heat is applied in the following ways:
a) Red heat Inoculating wires, points of forceps and searing spatulas are sterilized by holding them in the flame of a bunsen burner until they are seen to be red hot.
b) Flaming This method is used for sterilizing scalpels, needles, mouths of culture tubes, slides and cover slips. It involves passing the article through the bunsen flame without allowing it to become red hot.
c) Incineration This is an excellent method for destroying materials such as contaminated clothes, cotton wool stoppers, animal carcasses and pathological materials. It involves burning of materials in incinerators.
d) Hot air oven This is the most widely used method of sterilization using dry heat. The oven is usually heated by electricity and it has a thermostat that maintains the chamber air constantly at the chosen temperature.
It has a fan or turbo-blower to assist the circulation of air and to ensure rapid, uniform heating of the load. In Hot Air Oven, the air is heated at a temperature of 160oC for one hour. Figure 4.1 shows laboratory hot air oven.
Double jacket chamber
Thermometer
Shelves
Temperature indicator valve
Double jacket door
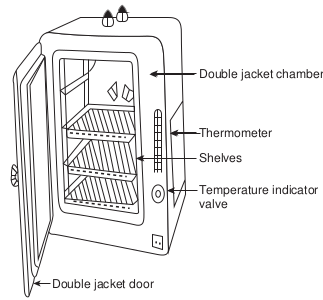
This is the best method of sterilizing dry glass ware such as test tubes, petri dishes, flasks, pipettes and instruments such as forceps, scalpels and scissors. It is also used to sterilize some pharmaceutical products such as liquid paraffin, dusting powder, fats and grease.
Quality control of dry heat sterilization: The spores of a nontoxigenic strain of Clostridium tetani are used to test the efficiency of dry heat sterlization. ### Sterilization by Moist Heat Moist heat kills microorganisms primarily by the coagulation of proteins (denaturation), which is caused by breakage of the hydrogen bonds that hold the proteins in three dimensional structure.
There are three methods employed in moist heat sterilization.
• Temperature below 100°C. • Temperature at 100°C. • Temperature above 100°C.
a) Temperature below 100°C: Pasteurization The process of heating a liquid food or beverage either at 62.8°C for 30 minutes or 72°C for 15 seconds to enhance their shelf life and destroy
Table 4.1: Comparison between Sterilization
Sterilization
Sterilized products have a longer shelf life
Discovered by Nicolas Appert
Eliminates all forms of microorganisms
Can be accomplished in many ways
Applied in food industry, medical, surgery and packaging
harmful microorganisms. It should be noted that pasteurization process kills only vegetative cells but not the spores. Pasteurization named in honour of its developer Louis Pasteur. Table 4.1 gives comparison between Sterilization and Pasteurization.
Raw milk can harbour dangerous m i c r o o r g a n i s m s , such as Salmonella, Escherichia coli and
Listeria, that can pose serious health risk, and children are particularly susceptible to the potential infection of unpasteurized or raw milk
Pasteurization can be done in the following methods,
• Low Temperature Holding Method (LTH) In this method milk, beer and fruit juices are maintained at 62.8°C for 30 minutes.
• High Temperature Short Time Method (HTST) Products are held at 72°C for 15 seconds.
• Ultra High Temperature (UHT)
and Pasteurization
Pasteurization
Pasteurized products have shorter shelf life
Discovered by Louis Pasteur
Eliminates pathogenic microorganisms only
Can be accomplished with heat
Mainly applied in food industry
| Steri liza ti on | Pas te uriza ti on |
|---|---|
| Ster i lize d p ro duc ts h ave a lo nger s helf lif e | Pasteur ize d p ro duc ts h ave s hor ter s helflif e |
| Di s co ver e d b y N ico l as A pp er t | Di s co ver e d b y L oui s P asteur |
| E limin ates a l l f or ms o f micr o orga ni sm s | E limin ates p at hog enicmicr o orga ni sm s o n ly |
| C an b e acco mpli she d in m any wa ys | C an b e acco mpli she d w it h h e at |
| Applie d in f o o d in dust r y, m e dic a l,sur ger y a nd p ac ka g in g | Main ly a pplie d in f o o d in dust r y |
Milk can be treated at 141°C for 2 seconds (This method employ temperature above 100°C).
b) Temperature at 100°C: i) Water at 100°C (Boiling): Boiling is one of the moist heat
sterilization methods. It kills vegetative forms of bacterial pathogens, almost all viruses and fungi (including their spores) within 10 minutes, usually much faster.
• Most vegetative bacteria will die in 5-10 minutes when immersed in boiling water, but some spores will survive at this temperature for several hours.
• Articles sterilized by this method cannot be stored for a long time.
ii) Steaming at 100°C (Tyndallization): It is a process discovered by John Tyndall
in 19th century for sterilizing substances to kill the spores of bacteria. The process of exposure of materials to steam at 100°C for 20 min for three consecutive days is known as tyndallization. First exposure kills all the vegetative forms and in the intervals between heating, the remaining spores germinate into vegetative forms which are killed on subsequent heating. Tyndallization is also called fractional sterilization or intermittent boiling.
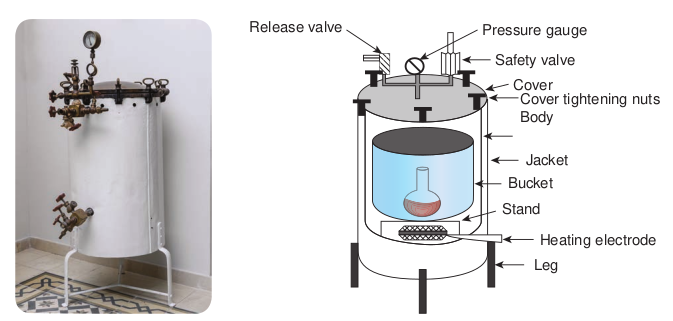
c) Temperature above 100°C: Moist heat sterilization can be carried out at temperature above 100°C in order to destroy bacterial endospores. This requires the use of saturated steam under pressure. This is achieved using autoclave.
Autoclave Sterilization using an autoclave is most effective when the organisms are either contacted by the steam directly or contained in a small volume of aqueous liquid (primarily water). The temperature used
in autoclave is 121°C at 15 lbs (pounds) pressure for 15 minutes (Figure 4. 2a & b).
Autoclaving is used in sterilizing culture media, instruments, dressings, applicators, solutions, syringes, transfusion equipment, pharmaceutical products, aqueous solutions and numerous other items that can withstand high temperatures and pressures. The same principle of autoclaving applies for the common household pressure cooker used for cooking food.
Factors influencing sterilization by heat: Sterilization by heat depends upon various factors such as time, temperature employed, number of microorganisms, spores and nature of material to be sterilized. Quality control of moist heat sterilization: To check the efficiency of moist heat sterilization, the indicator commonly used is the paper strips containing spores of Bacillus stearothermophilus.
Radiation
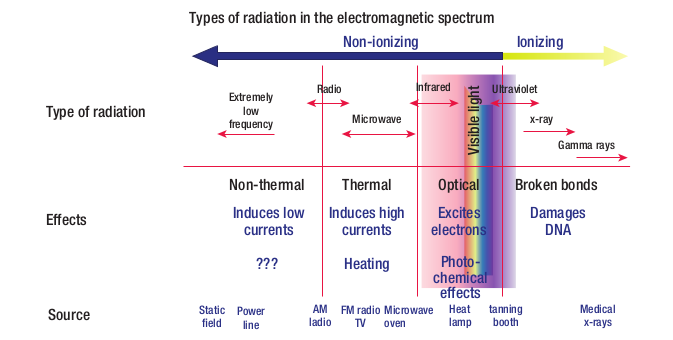
Radiation is commonly employed for sterilizing heat sensitive materials such as disposable plastic products and materials that cannot withstand moisture. The most effective type of radiation to sterilize or reduce the microbial burden in the substance is through the use of electromagnetic radiations. Figure 4.3 shows different types of electromagnetic radiations. Radiation has various effects on cells, depending on its wavelength, intensity and duration of explosure (Flowchart 4.2). Radiation that kills microorganism is of two types namely ionizing and nonionizing. a) Non-ionizing radiation Infra-red rays and ultra-violet rays are non ionizing radiation.
Source
Effects
Type of radiation Extremely
low frequency
Types of radiation in the e
Non-thermal
Induces low currents
In
???
Static field
Power line
AM ladio
Radio
Release valve
i) Infra-red radiation These are electromagnetic rays with wavelengths longer than those of visible light. These are low energy type. It kills microorganisms by oxidation of molecules as a result of heat generated. Infrared radiation is used for rapid mass sterilization of pre-packed items such as syringes and catheters.
in electromagnetic spectrum
Microwave x-ray
Gamma raysVi si
bl e
lig ht
lectromagnetic spectrum
Non-ionizing
duces high currents
Damages DNA
Heating
FM radio TV
Microwave oven
Heat lamp
tanning booth
Medical x-rays
Ionizing
Thermal Optical Broken bonds
UltravioletInfrared
Photo- chemical effects
Excites electrons
ve (b) Components of autoclave
Stand
Heating electrode
Bucket
Jacket
Cover tightening nuts Body
Cover
Safety valve
Pressure gauge
Leg
• Infrared radiation • UV radiation
• X-Rays • Gamma Rays
Ionizing radiationNon ionizing radiation
Radiation
Flowchart 4.2: Radiation
ii) Ultra-violet radiation The ultraviolet (UV) portion of the electromagnetic spectrum includes all radiations from 150-3900A°, UV radiation around 2600A° is most lethal to microorganisms. UV has a very little ability to penetrate matter. Thus, only the microorganisms on the surface of an object, exposed directly to the ultraviolet light are susceptible to destruction. UV radiations are used to sterilize operation theaters, laboratories and entry ways.
b) Ionizing radiation Ionizing radiations (X-rays, Gamma rays and Cosmic rays) are an excellent sterilizing agents and they penetrate deep into the objects. These radiations do not produce heat on the surface of materials. Hence, sterilization using ionizing radiations is referred as cold sterilization. It will destroy bacterial endospores and vegetative cells, both Prokaryotic and Eukaryotic; however ionizing radiation is not always effective against viruses. Gamma radiation from
Deinococcus radiodu- rans is an extremo- philic bacterium. It is one of the most radiation- resistant or-
ganisms known.
Cobalt 60 source is used in the cold sterilization of antibiotics, hormones, sutures and plastic disposables supplied such as syringes and in pasteurization of meat.
Filtration
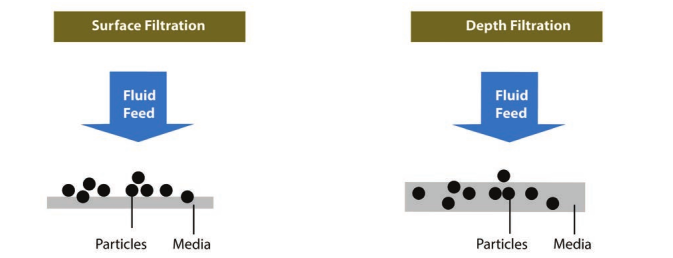
Filtration is an effective and reasonably economical method of sterilization. It is used to sterilize heat-sensitive fluids, and air. It is particularly useful for solutions containing toxins, enzymes, drug, serum and sugars. Sugar solutions used for the cultivation of microorganisms tend to caramelise during autoclaving and so they are best sterilized by filtration. Filtration is also used extensively in beer and wine industries. Filters with known pore sizes which are sufficiently small to hold back bacteria are employed. Recently filters that can remove viruses are also available.
Filtration is an excellent way to remove the microbial population from solution containing heat sensitive material.
There are two types of filters namely (Figure 4.4):
i) Membrane filter (surface filtration) and
ii) Depth filter
Membrane filters Membrane filtration is used for preparing heat-labile culture media components. It
iple of filtration
is also useful in removing bacteria from heat-sensitive pharmaceutical products and biological solutions.
Membrane filters are made up of either cellulose acetate, cellulose nitrate, polycarbonate, polyvinylidene fluoride or other synthetic porous materials. These filters remove microorganisms by screening them out, such as a sieve separates large sand particles from small ones. Membranes with pore size of 0.2µm in diameter are used to remove most vegetative cells but not viruses. These filters are used to sterilize pharmaceutical products, ophthalmic solutions, culture media, oils, antibiotics, and other heat sensitive solutions (Figure 4.5a, b & c).
Depth filters Depth filters are the oldest type of filters and they consist of overlapping layers of fibrous sheets of paper, asbestos or glass fibers. The overlapping fibers create
Sample to be filtered
Membrane transferred to culture medium
Membrane filter retains cells
(a)
(b)
(c)
To vacuum
Incubation
Colonies

microbial colonies
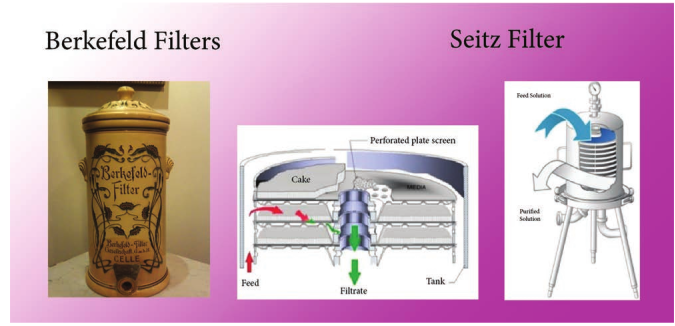
random paths through the filter that trap many particles. Depth filter are made up of diatomaceous earth (Berkefeld filters) which are used as water purifiers. Examples of types of depth filters (Figure 4.6) contains unglazed porcelain (Chamberl and filters) and asbestos (Seitz Filter).
Air filtration Air also can be sterilized by filtration.
2.5 mLM
ratus (b) Light microscope image of ne filter (c) Membrane filters showing on culture media
Give a reasonable method of sterilization for the following. 1. Operation theatre 2. Serum 3. Pot of soil 4. Plastic Petri Dishes 5. Rubber gloves 6. Disposable syringes. 7. Metal instruments 8. Flask of nutrient agar 9. Milk 10. Papers with spores.
HOTS
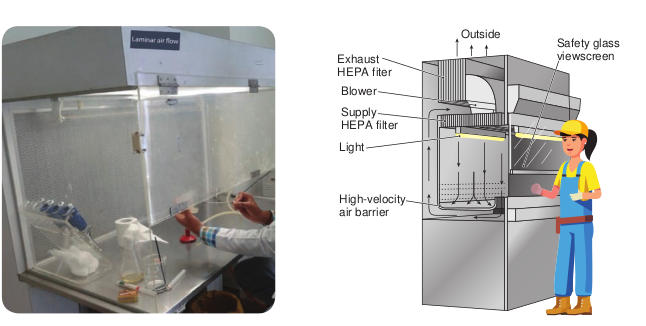
The air is freed from infection by passing it through High Efficiency Particle Arrester (HEPA) filter. Laminar air flow biological safety cabinets are one of the most important air filtration systems (Figure 4.7). It employes HEPA filters which remove 99.97% of 0.33µm particles
s of depth filters
Outside Safety glass viewscreenExhaust
HEPA fiter
Blower
Supply HEPA filter
Light
High-velocity air barrier
inar air flow
size. Some operation theaters and rooms occupied by burn patients receive filtered air to lower the numbers of airborne microbes. HEPA filters remove almost all microorganisms above 0.3µm in diameter.
Various physical methods of sterlization is summarized in Table 4.2
Table 4.2: Physical methods used to contr
Method Mechanism
of action C He
1 Dry a. Direct
flaming Burning contaminants to ashes
Very effe sterilizat
b. Incineration Burning to ashes
Very effe sterilizat
c. Hot –air sterilization
Oxidation Very effe sterilizat tempera about 1 h
2 Moi a. Boiling or
flowing steam
Protein denaturation
Kills veg and fung and almo within 1 effective
b. Autoclaving Protein denaturation
Very effe of steriliz 15 lbs of all vegeta their end killed in
c. Pasteurization Protein denaturation
Heat trea (72°C fo that kills and mos
3 Rad
a. Ionizing Destruction of DNA
Not wide routine s
b. Nonionizing Damage to DNA
Radiatio penetrat penetrat
ol microbial growth
omment Preferred for
sterilizing at
heat ctive method of ion
Inoculating loops
ctive method of ion
Paper cups, contaminated dressings, animal carcasses, bags, and wipes
ctive method of ion, but requires ture of 160°C for
our
Empty glassware, instruments, needles, and glass syringes
st heat etative bacterial al pathogens st all viruses
0 min; less on endospores
Dishes, basins, pitchers, various equipment
ctive method ation; at about pressure (121°C), tive cells and ospores are about 15 min
Microbiological media, solutions, linens, utensils, dressings, equipment, and other items that can withstand temperature and presure
tment for milk r about 15 sec) all pathogens t nonpathogens
Milk, cream, and certain alcoholic beverages(beer and wine)
iation
spread in terilization
Used for sterilizing pharmaceuticals and medical and dental supplies
n not very ing (non ing)
Control of closed environment with UV
| Me tho d | Me cha nis mof a c ti on | C omme nt | Prefe r re d fo rsteri lizin g | |
|---|---|---|---|---|
| He at | ||||
| 1 | Dr y he at | |||
| a. Dir e c tf l amin g | Bur nin gco nt amin antsto a she s | Ver y ef fe c t ive m et ho d o fster i liza t io n | Ino c u l at in g lo ops | |
| b. Incin era t io n | Bur nin g t oashe s | Ver y ef fe c t ive m et ho d o fster i liza t io n | Pap er c ups,co nt amin ate d dr es sin gs,anim a l c arc ass es, b ags,and w ip es | |
| c. Hot –a irster i liza t io n | Oxid at io n | Ver y ef fe c t ive m et ho d o fster i liza t io n, b ut r e quir estem p era tur e o f 160°C f orab out 1 h our | Em pt y g l asswa re,in st r um en ts, n e e d les,and g l ass sy r in ges | |
| 2 | Mois t he at | |||
| a. B oi lin g o rf lo w in gste am | Proteinden atura t io n | Ki l ls v eg et at ive b ac ter i a land f un ga l p at hog en sand a lm os t a l l v ir us esw it hin 10 min; les sef fe c t ive o n en dos p ores | Di shes, b asin s, p itcher s,va r io us e qui pmen t | |
| b. Auto cl av i ng | Proteinden atura t io n | Ver y ef fective methodof sterilization; at about15 lbs of pressure (121° C),all vegetative cells andtheir endospores arekilled in about 15 min | Micr obio log ic a l m e di a,s olut io ns, lin en s,uten si ls, dr es sin gs,e qui pmen t, a nd o t heritem s t hat c an w it hst andtem p era tur e a ndpre su re | |
| c. Pasteur iza t io n | Proteinden atura t io n | He at t re at men t f or mi l k(72°C f or a b out 15 s e c)t hat k i l ls a l l p at hog en sand m os t n onp at hog en s | Mi l k, cr e am, a ndcer t ain a lco holicb e vera ges(b e er a ndw in e) | |
| 3 | R adi ati on | |||
| a. Ionizin g | D es t r uc t io nof D NA | Not w ides pre ad inrout in e s ter i liza t io n | Us e d f or s ter i lizin gphar maceu t ic a ls a ndme dic a l a nd den t a lsupplies | |
| b. Nonio nizin g | D amage t o DNA | R adi at io n n ot v er yp en et ra t in g (n onp en et ra t in g) | C ont rol o f c los e denv ir onm en t w it h UV |
Summary Physical methods of microbial control include heat, radiation, drying and filtration.
Heat is the most widely used method of microbial control. It is used in both forms: moist and dry. The thermal death time (TDT) is the time required to kill all microbes at a specific temperature. The thermal death point (TDP) is the lowest temperature at which all microbes are killed in a specified duration of time.
Autoclaving, or steam sterilization, is the process by which steam is heated under pressure to sterilize a wide range of materials in a comparatively short time.
Dry heat kills the microorganisms under specified time and temperature. Dry heat is applied in the following ways: Red heat, incineration and Hot air oven.
Ionizing radiation (cold sterilization) by X rays and gamma rays is used to sterilize medical products and meat. It damages DNA and cell organelles by producing disruptive ions. Ultraviolet light, or nonionizing radiation, has limited penetrating ability. It is therefore restricted to sterilize suface of the materials.
Decontamination by filtration removes microbes from heat sensitive liquids and circulating air. The pore size of the filter determines what kinds of microbes are removed.
Evaluation Multiple choice questions
1. Which of the following does not kill endospores? a. Autoclaving b. Incineration
c. Hot-air sterilization d. Pasteurization
2. Which of the following is most effective for sterilizing Petri dishes? a. Chlorine b. Ethylene oxide c. Autoclaving d. Nonionizing radiation
3. kills organisms by coagulation and denaturing their proteins a. Dry heat b. Moist heat c. Both a & b d. None of the above
4. In which method, temperature of 160°C for 1 hour is employed? a. Red heat b. Infrared radiation c. Hot air oven d. Flaming
5. Which of the following temperature and time are employed in autoclave for sterilization of materials? a. 16 lbs 120°C for 18 min b. 18 lbs 180°C for 20 min c. 22 lbs 170°C for 35 min d. 15 lbs 121°C for 15 min
6. Wavelength used for the absorption of UV spectrum is a. 4000A° b. 2600A° c. 20A° d. None of the above
Answer the following
1. Define Pasteurization. 2. What is Incineration? 3. Define membrane filters? 4. What is Sterilization? 5. Explain the principle of moist heat
sterilization? 6. Differentiate the mechanism of
operation employed in autoclave and hot air oven.
7. Discuss ionizing radiation. 8. How do you sterilize heat sensitive
materials? 9. Define Tyndallization.
10. Describe the sterilization in an autoclave.
11. Explain the methods of sterilization by dry heat.
12. Explain the methods of radiation.
Student Activity
1. Collect samples of raw milk (unpasteurized) and boiled milk, place them in open containers separately. Observe the changes after a few hours in both and infer.
2. Making a working model of depth and membrane filters and demonstrating their uses.